Although digestive issues are not officially classified as direct symptoms of menopause, they are frequently reported during perimenopause and menopause. Bloating, constipation, stomach cramps—these are challenges many women face during this life stage, but why?
Digestive Issues and Menopause: An Overlooked Connection
When menopause is discussed, common symptoms like hot flashes and mood swings dominate the conversation. However, the gut often plays a silent role in the story. Hormonal shifts, stress, and age-related changes can all impact digestive health during menopause, leaving many women feeling frustrated and unsupported.
The Link Between Hormones and Gut Health
The interplay between hormones and gut health is profound, particularly during menopause, when significant hormonal fluctuations occur. Understanding these connections can shed light on why digestive issues become so prevalent during this stage of life.
Hormonal Fluctuations and Digestive Changes
During menopause, the body undergoes a dramatic decline in estrogen and progesterone levels. These hormones are not only essential for reproductive health but also play a critical role in maintaining digestive function:
- Estrogen: Helps regulate gut motility, the process by which food moves through the digestive tract. Lower levels can slow down this process, leading to constipation and bloating.
- Progesterone: Acts as a muscle relaxant. Its decrease can cause spasms or irregular contractions in the digestive tract, which may contribute to abdominal discomfort or irregular bowel movements.
These fluctuations can disrupt the delicate balance of the gut microbiome, causing symptoms such as:
- Persistent bloating.
- Alternating constipation and diarrhea.
- Increased sensitivity to certain foods.
The connection between hormones and gut health underscores why digestive changes are often one of menopause’s hidden symptoms.

Stress and the Gut-Brain Connection
Menopause often coincides with heightened levels of stress, which exacerbates digestive issues. The gut-brain axis, a bidirectional communication network between the brain and gut—plays a pivotal role here.
-
When stressed, the body activates its "fight or flight" response, redirecting energy from non-vital processes like digestion to deal with perceived threats. This can result in:
- Slower digestion, causing bloating and constipation.
- Increased gut sensitivity, leading to cramping or discomfort.
-
Emotional changes, such as anxiety and mood swings, common during menopause, can amplify this cycle. Stress alters gut microbiota composition, leading to dysbiosis—an imbalance in the gut bacteria that worsens symptoms.
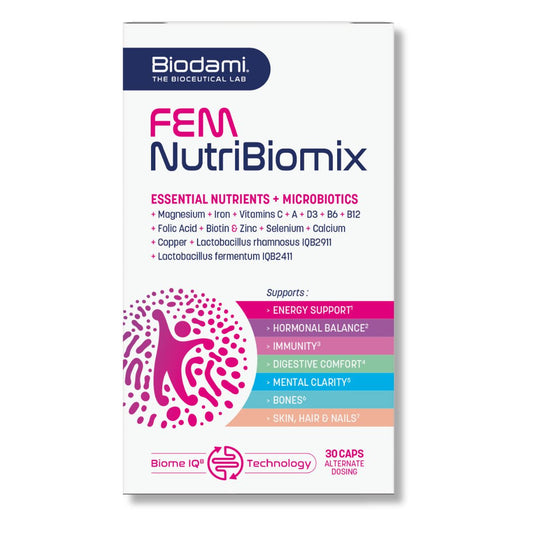
FEM NutriBiomix
- Precio habitual
- €29,95
- Precio de venta:
- €29,95
- Precio habitual
-
€89,85 - Precio unitario
- por