Investigating the link between stress and digestive symptoms
Stress is a normal part of life, but when it becomes chronic, it can take a toll on our physical and mental health. One area that is often affected by stress is the digestive system. In fact, stress and digestive symptoms have a complex and bidirectional relationship. Stress can affect digestion in several ways. When a person is stressed, the body releases hormones such as cortisol and adrenaline, which can lead to changes in the way the gut functions.
Research has shown that stress can lead to digestive symptoms, including abdominal pain, bloating, constipation, and diarrhea. Stress can also worsen existing digestive conditions such as irritable bowel syndrome (IBS) and inflammatory bowel disease (IBD). This is because stress triggers our brain to activate the sympathetic nervous system. This system is our body's "fight or flight" response, it prepares the body to protect itself against imminent danger by conserving functions that aren’t immediately needed for survival. That includes digestion. The emptying of the stomach is delayed, which can lead to a stomach-ache, indigestion, heartburn and nausea.
The gut and brain are connected by the gut-brain axis, a complex communication system that sends signals between the gut and brain. Stress can alter the gut-brain axis, which can lead to changes in the gut microbiome and further contribute to digestive symptoms.

On the other hand, digestive symptoms can also exacerbate stress. For example, if you have diarrhea or abdominal pain, you may be more likely to feel anxious or depressed. This can create a vicious cycle where stress leads to digestive symptoms, which then lead to more stress.
Additionally, stress can alter the balance of microorganisms in the gut, known as the gut microbiome. This can lead to a condition known as leaky gut, where the gut lining becomes more permeable, allowing harmful substances to pass through, which can lead to inflammation and an increased risk of infection.

Stress can also affect the appetite: it can lead to overeating or undereating.
It's important to note that not everyone will experience digestive problems when they are stressed, but some people may be more susceptible to it. Managing stress through techniques such as meditation, yoga, and exercise can help to improve digestion, as well as consulting with a healthcare professional if you are experiencing any symptoms.
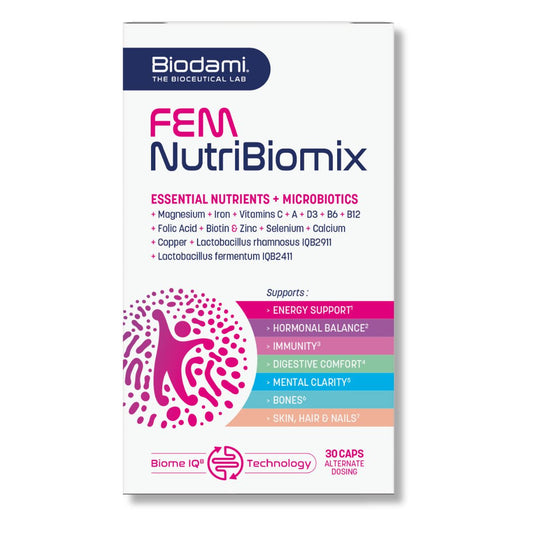
So, what can be done to break this cycle? One approach is to focus on stress management techniques, such as exercise, relaxation techniques, and therapy. Additionally, incorporating probiotics and other gut-supporting supplements into your diet can help to improve the gut microbiome and reduce inflammation in the gut. Studies have also shown that Ashwagandha, an adaptogen herb, can help the body to cope better with stress and improve overall well-being.

It's important to note that everyone's experience with stress and digestive symptoms is unique and individualized. If you are experiencing persistent digestive symptoms, it's important to consult with a healthcare professional to develop a personalized treatment plan.
Recommended For You
Sophie Cochez
Sophie is a biologist with a master’s degree in medical biology and additional training in microbiome science. Passionate about translating scientific knowledge into meaningful solutions, she founded Biodami to develop innovative, evidence-based supplements that support the microbiome and empower people to feel their best.
References
"Stress and the gut-brain axis: regulation by gut microbiota" by Lyte, M., Current Opinion in Microbiology, vol. 37, pp. 1-7, 2017.
"The gut-brain axis in irritable bowel syndrome" by Dunlop, S. P., et al, Neurogastroenterology & Motility, vol. 26, pp. 1615-1625, 2014.
"Ashwagandha (Withania somnifera) in the treatment of functional somatic syndromes and stress-related disorders" by Gupta, A., et al, Journal of Ayurveda and Integrative Medicine, vol. 8, pp. 12-19, 2017.
FIND OUT ABOUT OUR STRESS-GUT PROBIOTICS
Digest Stress RELAX
- Regular price
- €34,95
- Promotional price:
- €34,95
- Regular price
-
€104,85 - Unit price
- per